Introduction
Investments in health and health systems can create value in two distinct but related ways: by generating “value for money” and “value for many”.1 Policy makers have the opportunity to prioritize budgets in order to improve efficiency and effectiveness of health investments and expenditures thereby generating value for money, and target investments to improve equity and responsiveness to users’ needs, thereby achieving value for many.
The size of health budget and its allocation directly and indirectly impact on population health.2, 3 Low- and middle-income countries (LMICs) with similar per capita Gross Domestic Products (GDP), health expenditures as a proportion of GDP, and per person expenditure on health have different health systems outcomes in relation to population health (such as life expectancy, infant mortality, maternal mortality), financial protection (impoverishing expenditures for example) and user satisfaction.4 Beyond improvements in health system outcomes (better population health, financial protection and user satisfaction) investing in health brings distinct economic benefits for countries 5-10 and political benefits for the policymakers who choose to prioritize health to benefit citizens of a country who have electoral power.
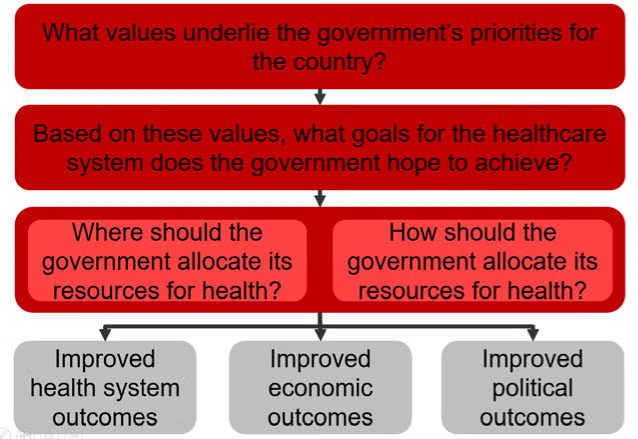
This article draws on a framework (Figure 1) used at Harvard University’s Ministerial Leadership in Health program, to discuss questions policymakers should consider when determining how to generate greater value by prioritizing health budgets. These questions include:
- What values underlie the government’s priorities for the country?
- Based on these values, what goals for the healthcare system does the government hope to achieve?
- Based on these goals, where should the government allocate its financial resources for health?
- How should the government allocate its financial resources for health?
These questions have direct relevance for Ministers of Health, Ministers of Finance, and other ministries whose decisions impact the health systems, and can provide a shared approach when discussing and setting priorities in order to achieve government goals.
Figure 1: Framework for aligning values and outcomes when setting priorities for health
What values underlie the government’s priorities for the country?
Although a broad range of values can drive the government’s approach to resource allocation, these value sets generally fall into three broad categories: utilitarian, liberal, and communitarian, discussed below.5, 11, 12
Utilitarians
Utilitarians are consequentialists and typically focus on the value, or utility, that a decision will have. Utilitarians generally believe “the ends justify the means” (assuming “the means” involve ethical and legal decisions). Policy tools such as cost-effectiveness and cost-benefit analysis reflect the utilitarian concerns of generating the greatest outcome for the greatest number of people using the fewest possible resources – ‘greatest good for the greatest number’. Utilitarians differ in how they choose to measure total utility. Subjective utilitarians argue that value is subjective to the individual and that individuals must directly judge their own happiness for themselves. In contrast, objective utilitarians argue that individual’s choices are not always rational and that greatest impact for the available resources can be achieved by defining (and measuring) individual well-being in objective terms (for example using a universal measure or index, such as Disability-Adjusted Life Years [DALYs] and Quality-Adjusted Life Years [QALYs] to objectively measure and compare everyone’s well-being) and by agents (such as policy makers, experts) and allocating resources to maximise these measure.
Liberals
Liberals take a rights-based approach to allocation of health resources. Liberals believe that all humans have the capacity and obligation to display mutual respect to each other, and this mutual respect endows individuals with rights. Some liberals, known as libertarians, focus on negative rights, which guarantee individual freedom. For example, libertarians might focus on the rights of the individual to buy health insurance or choose their physician. In contrast, egalitarian liberals also emphasize the importance of positive rights, or a minimum level of resources and services, which can guarantee the ability for an individual to exercise his or her free choices. Accordingly, egalitarian liberals tend to favor redistribution of resources in order to ensure that the entire population has access to basic positive rights. However, with regards to prioritizing health, egalitarian liberals differ in their views on whether individuals have a right to health services (i.e. provision of and access to care) or health status (i.e. the achievement of general well-being).
Communitarians
Communitarians do not focus on the level of the individual in assessing a policy, but rather on the level of the community or society. As such, communitarians evaluate the merit of a policy based on whether it adheres to a community’s value set and whether the policy promotes a society consistent with that value set. Communitarians would typically oppose a health policy which achieved positive population health outcomes with an intervention that defied local cultural norms or values. Communitarians fall into two broad categories: those who believe in a single set of values which would promote a better society (universal communitarians), and those who argue that each society should set its own values and norms based on the context-specific factors (relativist communitarians).
These value sets are not mutually exclusive. Policymakers might include both a utilitarian and communitarian perspective in an analysis where they prioritize health interventions based on their objective utility but exclude any that overtly defy local norms. Further, governments can modify their ethical values as they learn more about a population’s needs and their ability to meet those needs. However, it is important to maintain adequate “coherence and explicitness” when articulating one’s values; doing so creates transparency for the population and gives others the opportunity to agree with the government’s choices because they can understand the rationale behind these choices.
Based on these values, what goals for the healthcare system does the government hope to achieve?
Policymakers must consider which outputs and outcomes to prioritize when allocating resources for health. In this context, the term outputs refers to how well the health system performs its delivery of personal and public health services to the population, whereas outcomes, refer to the ultimate goals the health system aims to achieve. These goals include health status, financial protection, and user satisfaction. In many cases, strong delivery of health systems outputs is necessary but not sufficient for strong performance in relation to health system outcomes.
A policymaker needs to balance four key objectives for the outputs achieved by a health system:13
- Equity refers to the differences in how a policy affects people of different groups. An analysis of a policy’s “vertical equity” takes into account its differential impact across different populations (e.g. income or wealth levels, or different diseases), whereas an analysis of “horizontal equity” looks at whether the policy treats individuals at the same income level (or individuals that are similarly situated in relation to a health problem) the same.5
- Efficiency has been defined many ways in the fields of policy analysis. For the purposes of health systems analysis, we draw on economic definition of technical efficiency, in which society is producing the most goods and services for the least cost.5
- Effectiveness refers to whether interventions are evidence-based and safe.13 In other words, an effective intervention will achieve the desired health outcomes.
- Responsiveness refers to whether the health system meets the public’s legitimate non-medical expectations. Responsiveness is a highly subjective measure and depends on the perceptions among citizens of a health system’s functioning. 14
Policymakers’ values will influence which health system outputs they prioritize. For example, pure utilitarians will likely care most about efficiency and effectiveness, to achieve ‘value for money’, and they will less likely prioritize equity. They might also disregard the importance of responsiveness as an objective, unless they believe that a health system’s responsiveness generates value for the population. Liberals, who focus on individuals’ rights, will prioritize equity and responsiveness of the system, to achieve ‘value for many’, with libertarians emphasizing the importance of responsiveness (for example choice of health service providers) and egalitarian liberals emphasizing equity in access to positive rights (e.g. basic health services and medicines). Communitarians, who emphasize society’s values, will prioritize the objectives most relevant for achieving the best possible society. Accordingly, they will likely emphasize responsiveness and equity of the system at a societal level, although the emphasis could vary depending on the specific values of the society.
In addition to setting output objectives, policymakers must also pay attention to the health systems outcomes, or the overall goals, these outputs produce for a country’s health system: 5, 13
- Health status refers to the actual health of a population. Measurements of population health status include life expectancy, burden of disease, mortality rates for specific groups (e.g. infant mortality and maternal mortality), and prevalence of specific diseases.
- Financial risk protection refers to helping people avoid large and unpredictable payments for health, also known as catastrophic (or impoverishing) expenditures. Mechanisms to provide financial risk protection typically involve insurance schemes with risk-pooling functions, or tax funded health systems where services are typically ‘free’ or have low levels of cost sharing at the point of care delivery.
- Citizen satisfaction refers to the degree with which users of the health system rate the system as satisfactory.
As with outputs, health systems outcomes also derive directly from the values described earlier. For example, objective utilitarians might concern themselves most with the population’s average health status, whereas egalitarian liberals might focus most on the distribution or range of health statuses in the population (as a measure of equity levels). Egalitarian liberals will also emphasize the importance of financial risk protection as a means for ensuring economic opportunities for all. Subjective utilitarians might place a high value on citizen satisfaction, as would libertarians (in the sense that satisfaction relates to an individual’s level of choice.)
Based on these goals, where should the government allocate its financial resources for health?
Once the government has identified its objectives for the outputs and defined its goals for the health system, it can invest in specific programs or interventions accordingly. A health system has four main functions which a government can prioritize for investment: 13
- Governance and organization encompasses the organizations and institutions involved in delivering products and services to citizens15 such as hospitals, primary care clinics, and supply chains which provide medicines to providers. A government could choose to invest in the governance and organization of the health system by improving accountability, increasing transparency of decision making, updating management policies for health facilities, changing the referral network of the system, or improving processes for decision-making at the programmatic level.
- Health financing involves mobilizing, pooling and allocating financial resources. Funds can be mobilized through taxes, insurance or direct out-of-pocket payments, pooling could be achieved through pooling of contributions by the government or through insurance schemes – such as social health insurance, and community-based health insurance.3 A government could choose to invest in health financing by creating a new insurance scheme, expanding coverage of existing insurance to new patient populations, or by expanding the range of services covered under existing schemes. Finances can be allocated using budgets or other provider payment methods linked to individual patients (per capita payment), activity (fee-for-service or case mix payments), or outputs (performance related pay for achieving targets for example)
- Resource management entails overseeing the inputs, such as human resources and labor, pharmaceuticals, and medical technologies, that are used to produce outputs, for example provision of personal health care or public health services,. 15 The government can invest in the management of resources by purchasing these resources (e.g. by procuring medicines or by employing or contracting doctors), or by improving systems that oversee resources (e.g. budgeting tools, and health information systems) or that deliver them (e.g. through supply chain management systems) or by investing in infrastructure and human resources to strengthen health system by developing primary health care which enhances allocative and technical efficiency, improves population health outcomes at lower cost, achieves equity and improves user satisfaction. 16
- Personal healthcare and public health services refer to all of the activities actually involved in delivering care to patients. Strong health systems enable delivery of these services. Governments also invest in specific services that generate value for money and value for many – for example by investing in primary health care to deliver highly cost effective interventions that have population impact. Several investment cases have been made for “good buys” that can be delivered in an integrated manner at primary care level in an efficient and effective way, for example those identified by the Lancet Commission on Investing in Health 17; UNAIDS HIV Investment Framework 18; STOP TB Strategy 19; the Global Strategy for Women’s and Children’s Health spearheaded by the UN Secretary General 20; interventions identified in the Global Malaria Action Plan 21, and; the Package of Essential Noncommunicable Disease Interventions (also known as WHO-PEN) 22.
How should the government allocate its financial resources for health?
There is no formula for determining which health interventions or areas to prioritize, and while important limiting analyses to comparisons of cost-effectiveness is insufficient for policy making as values an priorities need to be considered carefully for each country.
Without universal consensus on the principles for prioritization, governments need to adopt an approach to make resource allocation decisions and justify their policies.23 Accordingly, ethicists at Harvard University have proposed a framework known as “accountability for reasonableness” (A4R) to guide this decision-making process. A4R which is a process grounded in democratic principles aimed at legitimizing decision-making among “‘fair-minded’ people who seek mutually justifiable terms of cooperation” has four conditions 24:
- Publicity condition: Decisions that establish priorities in meeting health needs and their rationales must be publicly accessible.
- Relevance condition: Policymakers should provide reasonable rationales which appeal to evidence, reasons, and principles accepted as relevant by fair-minded people when justifying their decisions. Rationale should be relevant for a broad range of stakeholders in decision-making.
- Revision and appeals condition: There must be mechanisms for challenge and dispute and, more broadly, opportunities for revision and improvement of policies in light of new evidence or arguments.
- Regulative condition: There must be public regulation of the process to ensure that conditions 1, 2, and 3 are met.
While A4R does not identify the priorities for government investments, it establishes a transparent deliberative process for publicly and legitimately determining these priorities in order to guide investment decisions. The principles of A4R have influenced priority setting for health in several places such as: UK, where the National Institute for Health and Clinical Excellence (NICE) takes social value judgments into account when making recommendations about coverage for new treatments 25; Mexico, where decisions about which diseases the public catastrophic insurance should cover involve working groups that evaluate the clinical, economic, ethical, and social considerations 26; and Oregon where, in 2008, a Health Fund Board made a plan to insure all legal residents of the state involving a wide group of stakeholders and extremely transparent decision-making / information-sharing 27.
The impacts of Government Health Spending
Health system outcomes
Changes in government health spending can directly impact on cause-specific mortality. For example, in low-income countries a 1% decrease in government health spending is associated with an increase of 18 deaths for every 100,000 live births in the neonatal period and 98 deaths before the age of five for every 100,000 live births, controlling for populations size, population structure, and inter-country differences in health care infrastructure. The statistical significance of this result holds even when controlling for economic conditions, infrastructure, infectious disease rates, and private health spending rates. 28
From 1999-2004, a 10% increase in per capita total health expenditure was associated with a 22% reduction in infant mortality rate and 10% increase in per capita public health expenditure was associated with a 21% infant mortality rate. 29 Globally, a 1% increase in government health spending is also associated with a significant decrease in cerebrovascular deaths.30
Increasing government health spending and improving the efficiency of spending can further overall life expectancy in a country. 9 For example, among nations below the regional average for GHS, increasing government health spending to the regional average would improve health adjusted life expectancy (HALE) by:
- 1.2 years in Africa
- 0.9 years in Asia / Pacific
- 4.1 years in Middle East / Central Asia
In addition, among nations below the regional average for efficiency in government health spending, increasing efficiency to the national average would result in an increase in HALE by:
- 1.5 years in Africa
- 1 year in Asia / Pacific
- 1.3 years in Middle East / Asia
Achieving the health systems goal of financial risk protection through universal health coverage (UHC) can also improve population health status. Cross-country analysis on the influence of insurance coverage on health outcomes suggests that financial coverage has a causal influence on health, especially for low-income individuals, who gain better access to necessary care when they receive coverage. 31
Examination of individual countries’ experiences implementing UHC supports this finding. For example, Thailand’s Universal Coverage Scheme included benefits such as inpatient and outpatient care, surgery, accident and emergency visits, dental care, diagnostics, prevention and health promotion, and medications, and universal coverage increased utilization of many health services, including inpatient and outpatient visits. 32, 33
Universal Health Coverage in Turkey rapidly expanded family medicine centered primary health care to improve ratio of nurses and physicians to patients across the country to address unequal distribution of human resources which helped to expand access to maternal and child health services, and resulted in a significant decrease in infant mortality and narrowed gaps in health outcomes between the rich and the poor. 13
Similarly, across many Latin American countries, where health has been established as a constitutional or legal right, several countries such as Brazil have expanded primary care as part of the platform universal health coverage, for improving efficiency of health budgets and to achieve equitable access to healthcare services. 34 The expansion of universal health coverage has led to significant declines in infant mortality, under-5 mortality, and maternal mortality across most Latin American countries between 1990 and 2010. 34
Economic outcomes
Evidence strongly suggests that improved population health has positive economic impacts for a country. Government health spending positively impacts on population health, and provides a sound “return on investment” in the form of stronger economic output and economic growth for the country. Evidence for the linkage between health and increased economic output exists at both the microeconomic and macroeconomic level.
Box 1. Case study of investments in antiretroviral treatment
Expenditures on antiretroviral treatment for people living with HIV/AIDS provide a useful case study of a health investment with significant health and economic returns. 39 By the end of 2011, 3.5 million patients were receiving antiretroviral treatment co-financed by the Global Fund, and 80% of those patients lived in 20 African countries. The total cost of treating these patients from 2011 to 2020 was estimated at $14.2 billion. This health investment was projected to save up to 18.5 million life-years. Further, the investment was estimated to yield up to $34 billion in economic benefits (for a net benefit of up to $19.8 billion) through three primary channels: $31.8 billion in labor productivity improvements, $0.83 billion in orphan care costs averted, and $1.4 billion from the delay of end-of-life care.39
Microeconomic Impact
At the microeconomic level, better health can improve the financial prospects for individuals and households. 6 In particular, malnutrition, frequent illness, and an unstimulating home environment can limit the physical and cognitive development of a child. Conversely, proper nutrition and health allows for the adequate physical development of children and improved performance in school. Thus, investments at an early age “help to raise the potential for long-term academic and workplace success and lifelong well-being.” 6
Interventions targeting specific diseases and conditions, such as deworming for school children, iron supplements and iodine to treat malnutrition, and malaria prevention can all lead to improved education or income outcomes for individuals. 7 Among working individuals, illness can have direct, negative consequences for their income. The mechanisms linking ill health to reduced income and wealth include impoverishing health expenditures, reduced education opportunities, decreased productivity at work, long-term separation from the work force, and disengagement from other economic activities.
Macroeconomic Impact
Macroeconomic evidence also supports the idea that investing in health generates positive economic returns.7 In particular, there are four channels through which investments in health might improve the overall economic state of a country, corroborated by the microeconomic evidence described above:
- Labor Productivity: Ceteris paribus, a healthy workforce will have higher labor productivity than an unhealthy workforce due to increase energy and reduced illness-related absenteeism, whereas illness in an individual can lead to loss of income, impoverishing expenditures, reduced productivity and loss of employment.
- Educational Opportunities: A healthy population has increased educational opportunities, and education levels have a direct impact on income growth for a country.
- Savings and Working Years: Populations with high life expectancies will tend to save more for the future and likely will have more working years. These increased savings can lead to increased investable capital, an important driver of growth.
- Demographic Dividend: Health investments that change mortality rates and total fertility can lead to a “demographic dividend,” in which the ratio of working-age to non-working-age people in the country increases and productive capacity increases on a per capita basis. Assuming that the country has or can create certain conditions to enable productivity of this working-age group (e.g. proper educational opportunities), the country will experience a “demographic dividend” that leads to its growth. This demographic dividend accounts for up to one-third of the economic boom that many East Asian countries experienced between 1965 and 1990.
Political outcomes
The process of formulating health policy and allocating resources to health depends on the political structure and climate of a country, and, as such, has implications for the country’s political outcomes. For example, the transition towards universal health coverage (UHC) has had distinct positive political benefits in many countries over the last several decades. 35 In addition, health policy in countries such as Turkey, the UK and Brazil has significantly influenced political landscape and political outcomes.
In Turkey, after a regime change in 2002, the government implemented a Health Transformation Program (HTP) with significant commitment from the political leadership of the country, and this transformation led to increased levels of public satisfaction with the government (Box 2) 13, 36 and have influenced voter intentions in favour of the government.i
After the re-democratization of the Brazilian government, the 1988 constitution formally defined health as a “citizen’s right and obligation of the state” and established the Unified Health System (SUS), which sought to unify the fragmented care delivery network into a national health system under the purview of the MoH. 37 Today, 75% of Brazil’s population, or 195 million people, receive services and coverage from SUS. 38
Box 2: Turkey’s Health Transformation Program
In the 1990s, Turkey faced three distinct but related problems related to its health system: inadequate and inequitable financing of the system, an absolute shortage and inequitable distribution of physical infrastructure and human resources, and disparities in health outcomes, especially between the east and west.13 Under-5 mortality rates in 1998 were 75.9 deaths per 1000 live births in the less-developed east and 38.3 deaths per 1000 live births in the more developed west. A major earthquake in 1999 left 17,000 dead and another 500,000 homeless, exposing major faults in the government’s ability to respond to emergencies and deliver services.
Turkey’s 2002 elections resulted in a majority for the Justice and Development Party, ending a decade of ineffective coalition governments. In 2003, as part of a broader objective to improve the economy and welfare, the Ministry of Health (MoH) introduced a Health Transformation Program (HTP) to help achieve UHC. Motivation to enact these changes, including improvements in the health system, came directly from public pressure, and a failure to achieve these goals would have resulted in public backlash. 36 Further, the public expressed high levels of dissatisfaction with the health system, with only 39.5% of people indicating they were satisfied with quality of care in 2003. Accordingly, the government displayed high levels of political commitment to this effort, with the Minister of Health visiting 81 provinces at the beginning of the HTP to meet with local government and agree to HTP implementation plans.
The HTP aimed to address several health system challenges, including organization, financing, service delivery, human resources, and pharmaceuticals. The government adopted a flexible approach when implementing HTP, combining incremental and tactical changes, with high visibility to citizens, with long-term, strategic shifts that required structural changes to the system. A transformation team continuously monitored progress of the HTP; with an emphasis on citizen satisfaction with the transition, conducting focus groups, stakeholder analyses, and annual household surveys.
The HTP led to significantly improved access to and usage of health services, resulting in improved health outcomes on a number of important measures such as infant and maternal mortality. User satisfaction with quality of care also increased to 79.5% by 2011. The successful rollout of HTP served as a blueprint for the expansion of other social services by the Turkish government, and public satisfaction with the process contributed to the government’s re-election in subsequent years.
i See for example Esen B. Myths and facts about Turkey’s welfare regime. Sabah. http://www.dailysabah.com/opinion/2014/08/26/myths-and-facts-about-turkeys-welfare-regime (Accessed April 7, 2016)
The UK Experience
In the UK, the National Health Service (NHS) receives broad public support, with 89% of the public agreeing with the idea of a tax-funded national health system, which is managed by the government. However, projections show that by 2030, the NHS will have a £65 billion funding gap. Therefore, UK policymakers will have to balance the competing health, financial, and social demands placed on the NHS in order to maintain its relevance going forward.
Conclusion
This article aims to introduce a framework for policymakers to consider how their values influence priority setting for health, and the potential impacts that these priorities will have on health systems, economic, and political outcomes.
By clearly articulating values and priorities, policymakers can develop a transparent and deliberative process to better discuss and engage their constituents in health systems decisions and to set priorities that create greater value for money by improving efficiency and effectiveness of budget allocation decisions and more value for many by enhancing equity and responsiveness in the health system.
References
- Atun, R., The National Health Service: value for money, value for many. Lancet, 2015. 385(9972): p. 917-8.
- Etienne, C., A. Asamoa-Baah, and D.B. Evans, Health systems financing: The path to universal coverage. 2010: World Health Organization.
- Gottret, P.E. and G. Schieber, Health financing revisited: a practitioner’s guide. 2006: World Bank Publications.
- The World Bank. Indicators. 2015 [cited 2015 March 23]; Available from: http://data.worldbank.org/indicator. http://data.worldbank.org/indicator
- Roberts, M., et al., Getting health reform right: a guide to improving performance and equity. 2008: Oxford university press.
- Jack, W. and M. Lewis, Health investments and economic growth: Macroeconomic evidence and microeconomic foundations. World Bank Policy Research Working Paper Series, Vol, 2009.
- Bloom, D. and G. Fink, The economic case for devoting public resources to health. Manson’s Tropical Diseases, 2013: p. 23-30.
- Atun, R. and S. Fitzpatrick, Advancing Economic Growth: Investing In Health. A summary, 2005.
- Grigoli, F. and J. Kapsoli, Waste not, want not: the efficiency of health expenditure in emerging and developing economies. 2013.
- Cutler, D.M., A.B. Rosen, and S. Vijan, The value of medical spending in the United States, 1960–2000. New England Journal of Medicine, 2006. 355(9): p. 920-927.
- The World Bank. How do national health systems reflect the country’s and the community’s values? 2011 [cited 2015 December 7].
- Roberts, M.J. and M.R. Reich, Ethical analysis in public health. The Lancet, 2002. 359(9311): p. 1055-1059.
- Atun, R., et al., Universal health coverage in Turkey: enhancement of equity. The Lancet, 2013. 382(9886): p. 65-99.
- World Health Organization, The World health report: 2000: Health systems: improving performance. 2000.
- Hsiao, W.C., Abnormal economics in the health sector. Health policy, 1995. 32(1): p. 125-139.
- Atun RA. “What are the advantages and disadvantages of restructuring a health care system to be more focussed on primary care services?” WHO Health Evidence Network. World Health Organization Regional Office for Europe, Copenhagen. 2004 http://www.euro.who.int/en/what-we-do/data-and-evidence/health-evidence-network-hen/publications/pre2009/what-are-the-advantages-and-disadvantages-of-restructuring-a-health-care-system-to-be-more-focused-on-primary-care-services
- Jamison, D.T., et al., Global health 2035: a world converging within a generation. The Lancet, 2013. 382(9908): p. 1898-1955.
- Schwartländer, B., et al., Towards an improved investment approach for an effective response to HIV/AIDS. The Lancet, 2011. 377(9782): p. 2031-2041.
- Raviglione, M.C. and M.W. Uplekar, WHO’s new Stop TB Strategy. The Lancet, 2006. 367(9514): p. 952-955.
- Ki-Moon, B., Global strategy for women’s and children’s health. New York: United Nations, 2010.
- Roll Back Malaria, The global malaria action plan. Roll Back Malaria partnership, 2008.
- World Health Organization, Package of essential noncommunicable (PEN) disease interventions for primary health care in low-resource settings. 2010.
- Daniels, N., Accountability for reasonableness: Establishing a fair process for priority setting is easier than agreeing on principles. BMJ: British Medical Journal, 2000. 321(7272): p. 1300.
- Gruskin, S. and N. Daniels, Process is the point: justice and human rights: priority setting and fair deliberative process. American Journal of Public Health, 2008. 98(9): p. 1573.
- Daniels, N. and J.E. Sabin, Accountability for reasonableness: an update. BMJ, 2008. 337.
- Daniels, N., Accountability for Reasonableness in Developing Countries, in Just Health: Meeting Health Needs Fairly. 2007, Cambridge University Press: Cambridge.
- Daniels, N., Decisions about access to health care and accountability for reasonableness. Journal of urban health, 1999. 76(2): p. 176-191.
- Maruthappu, M., et al., Government Health Care Spending and Child Mortality. Pediatrics, 2015: p. peds. 2014-1600.
- Anyanwu, J.C. and A.E. Erhijakpor, Health Expenditures and Health Outcomes in Africa*. African Development Review, 2009. 21(2): p. 400-433.
- Maruthappu, M., et al., Unemployment, government healthcare spending, and cerebrovascular mortality, worldwide 1981–2009: an ecological study. International Journal of Stroke, 2015.
- Moreno-Serra, R. and P.C. Smith, Does progress towards universal health coverage improve population health? The Lancet, 2012. 380(9845): p. 917-923.
- Hanvoravongchai, P., Health financing reform in Thailand: toward universal coverage under fiscal constraints. 2013.
- Limwattananon, S., et al., Why has the Universal Coverage Scheme in Thailand achieved a pro-poor public subsidy for health care? BMC Public Health, 2012. 12(Suppl 1): p. S6.
- Atun, R., et al., Health-system reform and universal health coverage in Latin America. The Lancet, 2014.
- Yates, R. and G. Humphreys, Arguing for universal health coverage.
- Atun, R. and S. Sparkes, Fixing a Broken Health System: Confronting Health System Challenges in Turkey. Harvard School of Public Health: Executive and Continuing Professional Education: Boston, MA.
- Couttolenc, B. and T. Dmytraczenko, Brazil’s primary care strategy. 2013.
- Kepp, M., Upcoming election could rekindle health debate in Brazil. The Lancet, 2014. 384(9944): p. 651-652.
- Resch, S., et al., Economic returns to investment in AIDS treatment in low and middle income countries. PloS one, 2011. 6(10): p. e25310.